Torn Meniscus - Repair and Post Op Instructions
What is a Meniscus?
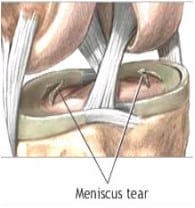
The Medial and Lateral meniscal cartilages are gasket like cushions in the knee. Positioned between the femur and tibia, they distribute the weight transferred from the larger femur above to the smaller tibia below. The Menisci also help with the stability of the knee joint. Healthy Menisci convert the relatively flat tibial surface into a more stable shallow socket
Why Do They Tear?
Meniscal tears can occur in any age group. In younger people, the meniscus is a fairly tough and rubbery structure. Tears in the meniscus usually occur as a result of a forceful twisting injury or with hyperflexion of the knee. In younger age groups, meniscal tears are more likely to be caused by a sports injury. In more mature individuals, it can occur with squatting down, twisting or a fall. In older individuals, the meniscus can be weaker and easier to tear. Sometimes meniscal tears can occur as a result of a minor injury, even from the up and down motion of simple squatting. Degenerative tears of the meniscus can also be seen as a part of osteoarthritis of the knee, gout and other arthritic conditions.
In many cases, knee pain is the most common complaint and the patient cannot recall one clear associated injury that leads to the meniscus tear. The pain may be felt along the joint line where the meniscus is located. Sometimes the symptoms are much more vague and occasionally they involve the whole knee. If the torn portion of the meniscus is large enough, locking may occur. Locking simply refers to the inability to fully straighten the knee or loss of the ability to move the knee. Locking occurs when a piece of torn cartilage, or meniscus, is stuck between the bones (see the picture above). In other words, the meniscus is caught in the hinge mechanism of the knee. Once stuck, it will not let the knee straighten out or move completely. (To see Dr. Reznik’s video, “The Locking Knee”, go to Youtube.com/DrAReznik.)
Left alone, over time the locking and/or constant rubbing of the torn meniscus on the articular cartilage will cause damage or degeneration of the knee joint. As a result, the knee may also become swollen, stiff and tight.
Treatment: Meniscal Repair
Once a meniscus is torn, it won’t heal on its own. The tear can be treated safely with an Arthroscopic procedure that Dr. Reznik performs as an outpatient. It is often done under a light anesthetic with a local injection for post operative comfort. When the tear is repaired, Dr Reznik uses the arthroscope to place tiny sutures or stitches to fix the tear. Of the tears below the ones nearest the outer edge are more often repaired, depending on the overall condition of the cartilage. That is where the blood supply is best and the cartilage has the best chance of healing (the first, second and fourth images below). Radial tears (image eight below) can be repaired on rare occasions.

Meniscal Recovery Plan
Diet: You may resume a regular diet when you return home. Start with tea or broth and advance slowly with crackers or toast, then a sandwich. If you become nauseated, return to clear liquids.
Pain Control: Take pain medication as prescribed by Dr. Reznik. Please call our office with any questions regarding your medication. Ice as needed (never place ice directly on skin) and elevate leg above heart level using 2-3 pillows. This will also decrease swelling.
Stop smoking: Smoking slows the healing process by interfering with the making of new DNA. Smoking also increases the risk of infection and pneumonia after surgery by slowing your body’s white blood cells.
Deep Breathing: Be sure to regularly take a deep breath and blow it out. This helps to clear the lungs after anesthesia.
Knee Immobilizer: Meniscal Repair patients are to wear the knee immobilizer full time for the first 3 weeks to protect the repair for the first phase of healing. This includes while you are sleeping. It is to be removed only for physical therapy directed exercises and showers.
Note: Patients should not flex the knee past 90 degrees for the first 3 weeks even if you therapist says it is okay. After 3 weeks, you will change from the immobilizer to a knee hinged brace. This is normally done by the physical therapist; if you or your therapist is unsure about what to use or when to change your brace call Dr. Reznik’s office. Under guidance, you can then start bending the knee from 90 degrees to a maximum of 120 degrees. When first switching to the knee hinge brace, you may need to use two crutches again for a short time to help with balance if needed.
Crutches: Patients are to use two crutches for the first week, putting light weight on the operative leg with each step with the immobilizer on. Remember to put the involved foot flat on the ground. Most patients can be fully weight bearing by the end of the first week while continuing to wear the immobilizer. After the first week, you may then increase weight as tolerated and advance to one crutch for a few days and then a cane if needed. Meniscus (cartilage) Repair patients cannot do twisting, pivoting, squatting, deep knee bends or impact activities for four months. It is vital that meniscus repair patients do not squat for at least four months after the repair.
Return to Work: People with light work (like desk or computer work with no squatting, lifting or kneeling) can return to work within a week to ten day with the brace on. The exception is for people who may have long commutes. By staying still with the leg down for long periods, increases the risk of a BLOOD CLOT in the leg. Patients with active office work or very light labor with variable tasks can sometimes go back to work at two or three weeks, depending on lifting requirements and if their employer will make accommodations for light duty. Heavy work, (lifting or unprotected heights) cannot usually return before 6 weeks. Most will need to be cleared by their physical therapist. The heaviest of labor, working in unprotected heights would naturally take longer. Driving: Right knee patients and left knee patients with a standard transmission car cannot drive until out of the knee immobilizer, off all pain meds and can fully weight bear without pain. Left knee surgery patients can drive after 3 weeks if they have no pain and you are off pain all pain medications comfortable walking without crutches.
Blood Clots: Those at higher risk of blood clots include those patients who have sedentary life styles, long car or train commutes, have a history of prior cancer, women on birth control pills, may be overweight or males over the age of 40. These patients should be taking an at least a baby aspirin per day (unless allergic or sensitive). Doing the exercises (ankle pumps below), using aspirin and at times compressive stockings will also reduce the risk of blood clots. Patients who have a history of clots in the past or three or more of the above risk factors should ask if they should be on a blood thinner post op for at least six weeks.
Call the Physician If:
- You develop excessive, prolonged nausea or vomiting
- Fever above 101
- You develop any type of rash
- You experience calf pain
Post-Operative Exercises: Start doing exercises while still in the recovery room. Dr. Reznik or your nurse will instruct you on what to do. At home, while resting in bed after surgery do the following every hour or with each set of TV commercials.
Ankle Pumps: Pump your ankle up and down for 1 minute (like pressing on the gas pedal). This will increase circulation and reduce the risk of developing a blood clot. If watching TV, do this during every commercial.
Straight Leg Raise: Tighten your quads (muscle in the front of your thigh) with the knee immobilizer on and raise your leg 8 to 12 inches off the bed. Do at least three times a day.
Add other exercises as your therapist gives them to you.
Knee bends/heel slides: With your heel on the bed, bend your knee while sliding your heel toward you. Start with bending 30-45 degrees and work toward 90 degrees during the first week.
If you are in bed for extended periods, move your arms regularly. Use light weights for upper arm exercises and keep muscle tone for using crutches.

